Health care helpline
Health Care & Insurance
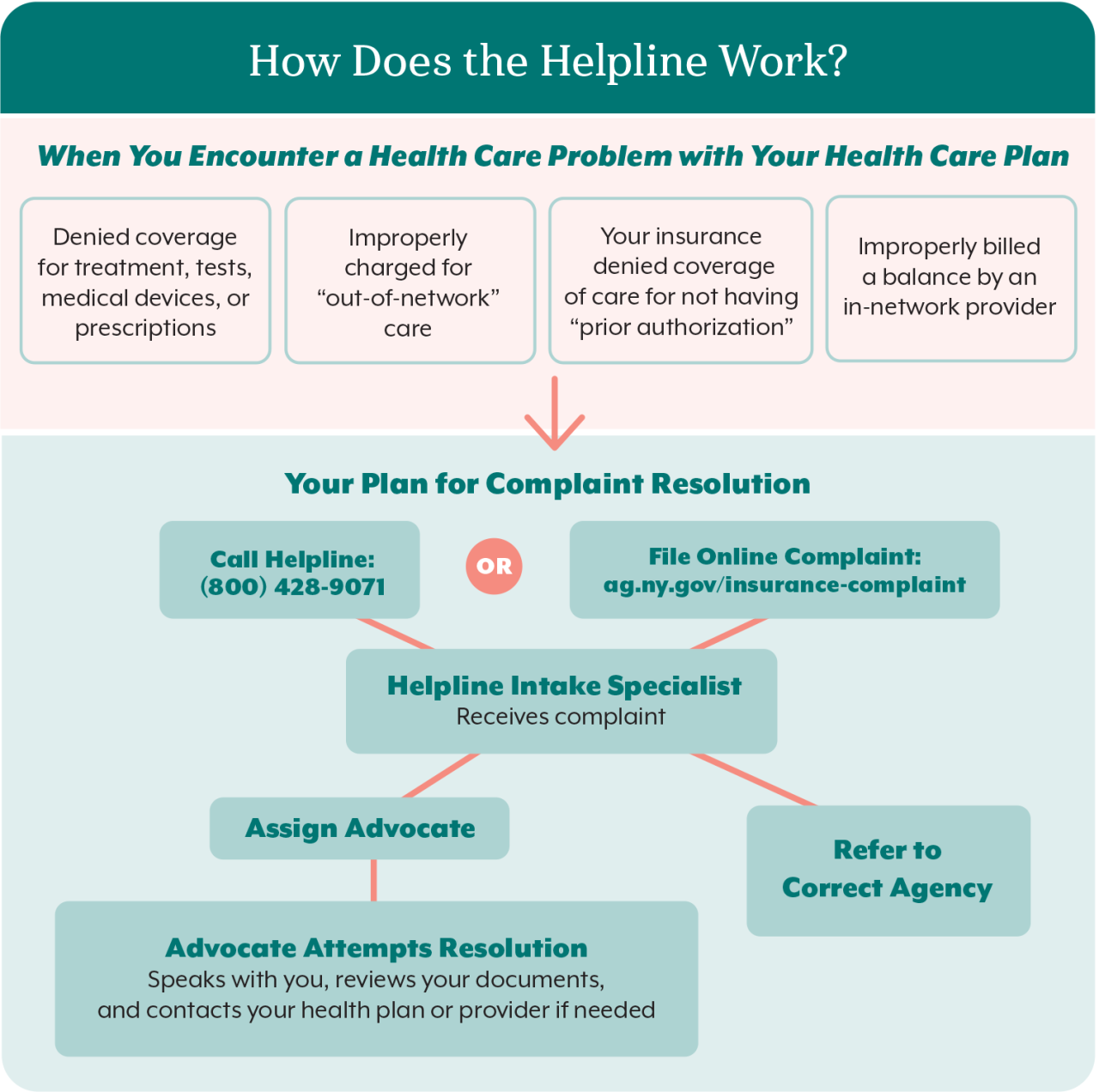
How does the helpline work?
We can help when you encounter a problem with your health care plan:
- You are denied coverage for treatment, tests, medical devices, or prescriptions.
- You are improperly charged for "out-of-network" care.
- Your insurance is denied coverage of care for not having "prior authorization."
- You are improperly billed a balance by an in-network provider.
Here is your plan for complaint resolution:
- You call the helpline at 1-800-428-9071 or file an online health care complaint
- A helpline intake specialist receives your complaint and assigns an advocate or refers the complaint to the appropriate agency
- The advocate attempts resolution by speaking with you and reviewing your documents. The advocate contacts your health plan or provider if needed
Tips for faster complaint resolution
What documents should I gather?
Find guidance on how to file an appeal and information about time limits on your explanation of benefits (EOB), denial notice, and health plan documents.
Can my provider help?
Your provider's office may be able to resubmit your claim, appeal the denial of coverage, provide medical records, or write a letter in support of an appeal.
What should I document?
Document everything. Keep a copy of everything you send to your insurer or receive from them. Keep written notes of conversations, including the date, the person you spoke to, and what was said.
My health insurance plan denied a claim. What can I do?
You have a right to know why a claim was denied and to appeal that decision. Ask your health insurer to review its decision through the internal appeal process, which often includes two levels of appeal.
Why was I denied coverage by my health insurance plan?
Review your explanation of benefits (EOB), or your notice of denial. The EOB is a statement sent by your health insurance company explaining what it will cover and any costs you may have to pay out of pocket. It is sent after your doctor submits a claim. You may also call your health plan for an explanation.
When must I appeal?
Plans have different time limits and rules for appealing. Act quickly.
My insurer sent me a denial letter. What else can I do?
If your internal appeal fails, you may have other options, depending on your type of health plan and the type of denial. You may have the right to make an external appeal to the New York State Department of Financial Services for an independent review by a medical professional.
You can generally challenge the following:
| Problem | What to do |
| No prior authorization: Your health insurance plan requires your doctor to get approval for certain medicines, tests, medical devices, or procedures before it will pay for the cost. | Ask your doctor to request prior authorization, showing the care or medication you are seeking is medically necessary or that you meet the requirements for approval. |
| Not a covered benefit: A medication, test, procedure, or specific care isn’t covered by your plan. | Double check your benefits in your member handbook and push for coverage where exclusions are vaguely worded or the plan documents could be interpreted to provide coverage for the denied service. |
| Not medically necessary or Investigational or experimental: Insurance plans will not pay for the care you are seeking because they find it not “medically necessary” or it doesn’t meet the accepted standards of good medical practice for treating your condition or disease. | Work with your doctor to obtain documents and other proof to explain to the plan that your treatment is medically necessary. |
| Out of network: You are denied coverage of treatment by a specialist or other provider outside of your plan’s network of doctors. |
Check your provider directory. If the doctor was mistakenly included, contact your insurer. If you were treated in the emergency room by an out-of-network doctor or if your primary physician referred you to a doctor who you did not know was out of network, New York law protects you. Contact your insurer. |
If you need help, contact us:
Health Care Bureau helpline: 1-800-428-9071 or online complaint form for a health care issue
