Criminal Justice Division
Criminal Enforcement and Financial Crimes Bureau
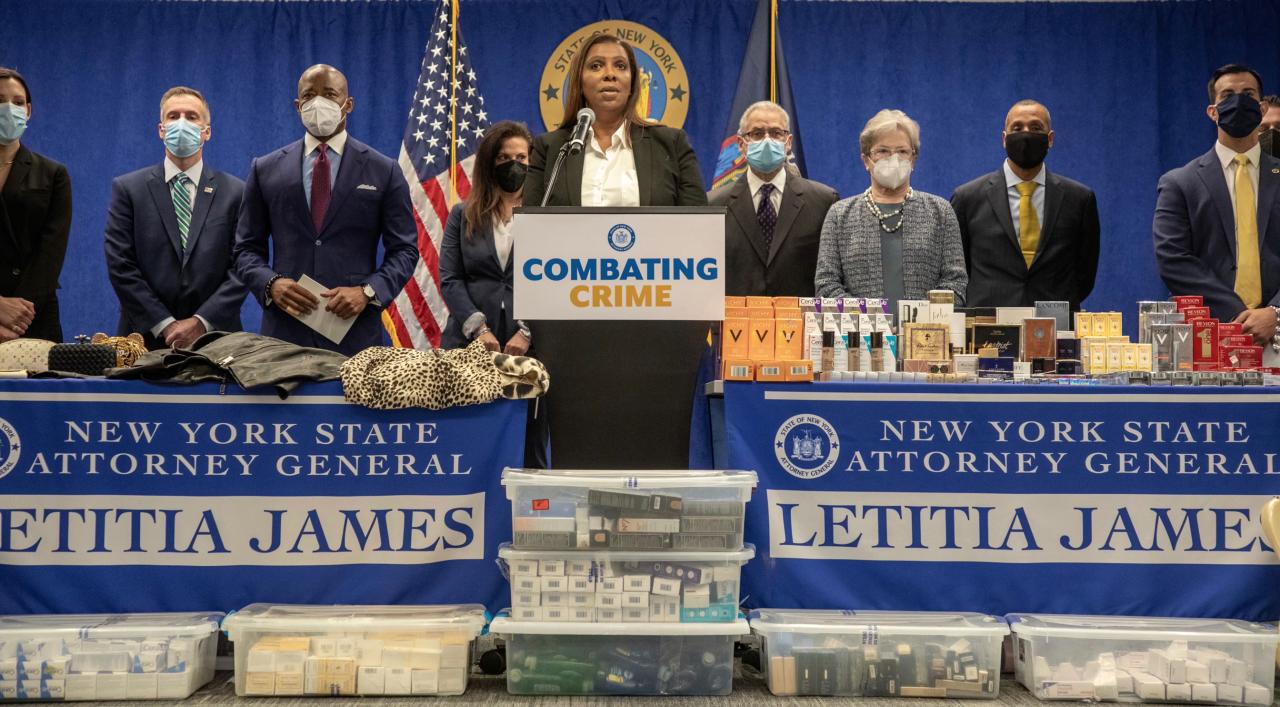
The Attorney General's unique statewide criminal jurisdiction enables the Criminal Enforcement and Financial Crimes Bureau to address criminal conduct throughout the state, including complex financial crimes that cross county lines.
Criminal Enforcement and Financial Crimes Bureau work
Investigations
Investigations consists of over 200 sworn police officer and civil investigators in the Major Investigations Unit, Criminal Enforcement and Financial Crimes Bureau, Medicaid Fraud Control Unit, Office of Special Investigations, Organized Crime Task Force, Public Integrity Bureau, and Special Operations Unit. Investigators assist with the office’s ongoing civil and criminal investigations and prosecutions. Many have specialized training in computer forensics; language; forensic accounting; and technical surveillance, such as through wiretaps, bugs, and cameras. Over 40 civil investigators are assigned to work on supporting a defense in lawsuits brought against state agencies and employees.
Medicaid Fraud Control Unit
The Medicaid Fraud Control Unit, the largest unit within the Attorney General’s Criminal Division, is the centerpiece of New York’s effort to investigate, penalize, and prosecute individuals and companies responsible for improper or fraudulent Medicaid billing schemes. It also handles numerous cases in order to safeguard elderly and disabled New Yorkers from abuse and neglect in nursing homes and other health care facilities.
Statewide Offices
Main Place Tower, Suite 300B
350 Main Street
Buffalo, New York 14202
716-853-8500
144 Exchange Boulevard, Suite 600
Rochester, New York 14614
585-262-2860
300 South State Street, Suite 350
Syracuse New York 13202
315-423-1104
The Capitol
Albany New York 12224
518-533-6011
28 Liberty Street
New York New York 10005
212-417-5300
300 Motor Parkway, Suite 210
Hauppauge, New York 11788
631-952-6400
One Blue Hill Plaza, Suite 1037
P.O. Box 1557
Pearl River, New York 10965
845-732-7500
Medicaid Fraud Control Unit work
Office of Special Investigation
OSI investigates every death in the State of New York that may have been caused by a police officer or a peace officer (peace officers includes corrections officers). If OSI concludes that an officer caused a death, OSI will either present evidence to a grand jury for consideration of criminal charges, or publish a report explaining why the evidence in the case does not warrant presentation to a grand jury. If a grand jury returns an indictment, OSI proceeds to prosecute the case.
Organized Crime Task Force
The Attorney General's Statewide Organized Crime Task Force (OCTF) was established by the Legislature in 1970 through the enactment of Section 70-a of the New York State Executive Law. OCTF is responsible for investigating and prosecuting multi-county, multi-state, and multi-national organized criminal activities occurring within the state.
Organized Crime Task Force work
Public Integrity Bureau
The Public Integrity Bureau investigates and supports the public's interest in honest government. When government actors, or private individuals acting in concert with them, engage in corruption, fraud, or illegal behavior in the course of their public duties, the bureau may investigate or take enforcement action to restore the public's interest in honest government and the integrity of officials at the state and local level. The bureau handles complex investigations into government corruption, fraud, and abuse of authority. Although part of the Criminal Justice Division, the bureau brings cases under both civil and criminal authority, and may also issue reports about its investigations and findings.
The Attorney General has made a top priority of cracking down on corruption and restoring the public’s trust in government. The office partners with the state Comptroller to investigate public corruption involving taxpayer funds. In addition, the Attorney General has designated public integrity officers in every region of the state to give New Yorkers a place to report complaints of government corruption without the fear of local politics influencing the outcome.
Public Integrity Bureau work
Real Estate Enforcement Unit
The Real Estate Enforcement Unit investigates complaints and prosecutes cases involving bank fraud, deceptive lending practices, deed theft, tenant harassment, and frauds committed upon city and state agencies by landlords, real estate developers, and others.
